What is Antibiotic Resistance and Why isresistance a global concern including Gambia
Antibiotic resistance occurs when an antibiotic has lost its ability to effectively control or kill bacterial growth; in other words, the bacteria are “resistant” and continue to multiply in the presence of therapeutic levels of an antibiotic.
With the discovery of antimicrobials in the 1940s, scientists prophesied the defeat of infectious diseases that had plagued humankind throughout history.However, the remarkable healing power of antibiotics invites widespread and often inappropriate use. This misuse and overuse of antibiotics leads to antibiotic resistance among bacteria and consequent treatment complications and increased healthcare costs.
Antimicrobial resistance has cast a shadow over the medical miracles we take for granted, undermining every clinical and public health program designed to contain infectious diseases worldwide.Limited access to medical care and effective treatments, the common practice of self-medication, and the availability of counterfeit drugs have exacerbated drug resistance in the developing world.In affluent nations, infections acquired in settings such as hospitals and nursing homes are a major source of illness and death. In addition, community-acquired infections are emerging, both as independent epidemics and as primary sources of resistance in hospitals.If resistance to treatment continues to spread, our interconnected, high-tech world may find itself back in the dark ages of medicine, before today’s miracle drugs ever existed.
WHO REPORT ON Antimicrobial resistance
Key facts
·Antimicrobial resistance threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses and fungi.
·It is an increasingly serious threat to global public health that requires action across all government sectors and society.
·Antimicrobial resistance is present in all parts of the world. New resistance mechanisms emerge and spread globally.
·In 2012, WHO reported a gradual increase in resistance to HIV drugs, albeit not reaching critical levels. Since then, further increases in resistance to first-line treatment drugs were reported, which might require using more expensive drugs in the near future.
·In 2013, there were about 480 000 new cases of multidrug-resistant tuberculosis (MDR-TB). Extensively drug-resistant tuberculosis (XDR-TB) has been identified in 100 countries. MDR-TB requires treatment courses that are much longer and less effective than those for non-resistant TB.
·In parts of the Greater Mekong sub region, resistance to the best available treatment for falciparum malaria, artemisinin-based combination therapies (ACTs), has been detected. Spread or emergence of multidrug resistance, including resistance to ACTs, in other regions could jeopardize important recent gains in control of the disease.
·There are high proportions of antibiotic resistance in bacteria that cause common infections (e.g. urinary tract infections, pneumonia, bloodstream infections) in all regions of the world.
·Patients with infections caused by drug-resistant bacteria are generally at increased risk of worse clinical outcomes and death, and consume more health-care resources than patients infected with the same bacteria that are not resistant.
What is antimicrobial resistance?
Antimicrobial resistance is resistance of a microorganism to an antimicrobial drug that was originally effective for treatment of infections caused by it.
Resistant microorganisms (including bacteria, fungi, viruses and parasites) are able to withstand attack by antimicrobial drugs, such as antibacterial drugs (e.g. antibiotics), antifungals, antivirals, and antimalarial, so that standard treatments become ineffective and infections persist, increasing the risk of spread to others.
Poor infection control practices, inadequate sanitary conditions and inappropriate food-handling encourage the further spread of antimicrobial resistance.
What is the difference between antibiotic and antimicrobial resistance
Antibiotic resistance refers specifically to the resistance to antibiotics that occurs in common bacteria that cause infections. Antimicrobial resistance is a broader term, encompassing resistance to drugs to treat infections caused by other microbes as well, such as parasites (e.g. malaria), viruses (e.g. HIV) and fungi (e.g. Candida).
Why is antimicrobial resistance a global concern
New resistance mechanisms emerge and spread globally threatening our ability to treat common infectious diseases, resulting in death and disability of individuals who until recently could continue a normal course of life.
Without effective anti-infective treatment, many standard medical treatments will fail or turn into very high risk procedures.
Antimicrobial resistance kills
Infections caused by resistant microorganisms often fail to respond to the standard treatment, resulting in prolonged illness, higher health care expenditures, and a greater risk of death.
As an example, the death rate for patients with serious infections caused by common bacteria treated in hospitals can be about twice that of patients with infections caused by the same non-resistant bacteria. For example, people with MRSA (methicillin-resistant Staphylococcus aureus, another common source of severe infections in the community and in hospitals) are estimated to be 64% more likely to die than people with a non-resistant form of the infection.
Antimicrobial resistance hampers the control of infectious diseases
Antimicrobial resistance reduces the effectiveness of treatment; thus patients remain infectious for a longer time, increasing the risk of spreading resistant microorganisms to others. For example, the emergence of Plasmodium falciparummultidrug resistance, including resistance to ACTs in the Greater Mekong subregion is an urgent public health concern that is threatening global efforts to reduce the burden of malaria.
Although MDR-TB is a growing concern, it is still largely under-reported, compromising control efforts.
Antimicrobial resistance increases the costs of health care
When infections become resistant to first-line drugs, more expensive therapies must be used. A longer duration of illness and treatment, often in hospitals, increases health care costs as well as the economic burden on families and societies.
Antimicrobial resistance jeopardizes health care gains to society
The achievements of modern medicine are put at risk by antimicrobial resistance. Without effective antimicrobials for prevention and treatment of infections, the success of organ transplantation, cancer chemotherapy and major surgery would be compromised.
Present situation
Resistance in bacteria
Resistance in tuberculosis
In 2013, there were an estimated 480 000 new cases of MDR-TB in the world. Globally, 3.5% of new TB cases and 20.5% of previously treated TB cases are estimated to have MDR-TB, with substantial differences in the frequency of MDR-TB among countries. Extensively drug-resistant TB (XDR-TB, defined as MDR-TB plus resistance to any fluoroquinolone and any second-line injectable drug) has been identified in 100 countries, in all regions of the world.
Resistance in malaria
The emergence of P. falciparum multidrug resistance, including resistance to ACTs, in the Greater Mekong subregion is an urgent public health concern that is threatening the ongoing global effort to reduce the burden of malaria. Routine monitoring of therapeutic efficacy is essential to guide and adjust treatment policies. It can also help to detect early changes in P. falciparum sensitivity to antimalarial drugs.
Need for concerted actions
Antimicrobial resistance is a complex problem driven by many interconnected factors. As such, single, isolated interventions have little impact. Coordinated action is required to minimize emergence and spread of antimicrobial resistance.
People can help tackle resistance by:
hand washing, and avoiding close contact with sick people to prevent transmission of bacterial infections and viral infections such as influenza or rotavirus, and using condoms to prevent the transmission of sexually-transmitted infections;
getting vaccinated, and keeping vaccinations up to date;
using antimicrobial drugs only when they are prescribed by a certified health professional;
completing the full treatment course (which in the case of antiviral drugs may require life-long treatment), even if they feel better;
never sharing antimicrobial drugs with others or using leftover prescriptions.
Health workers and pharmacists can help tackle resistance by:
enhancing infection prevention and control in hospitals and clinics;
only prescribing and dispensing antibiotics when they are truly needed;
prescribing and dispensing the right antimicrobial drugs to treat the illness.
Policymakers can help tackle resistance by:
improving monitoring around the extent and causes of resistance;
strengthening infection control and prevention;
regulating and promoting appropriate use of medicines;
making information widely available on the impact of antimicrobial resistance and how the public and health professionals can play their part;
Rewarding innovation and development of new treatment options and other tools.
Policymakers, scientists and industry can help tackle resistance by:
Fostering innovation and research and development of new vaccines, diagnostics, infection treatment options and other tools.
For further information www.gcc.gm www.consrumerinternatiaonal.org, email azadehhassan@yahoo.co.uk, Text Dr Azadeh 002207774469,3774469
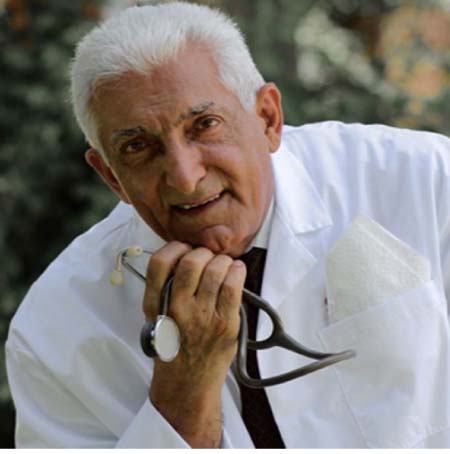
Author DR AZADEH Senior Lecturer at the University of the Gambia, Senior Consultant in Obstetrics & Gynaecology, Clinical Director of Medicare Health Services.




