Miscarriage (losing pregnancy)
PREVENTION, CAUSES, SYMPTOMS, TREATMENT
What is a miscarriage?
A miscarriage is the spontaneous loss of a pregnancy from conception to 20 weeks’ gestation. The term stillbirth refers to the death of a foetus after 20 weeks’ gestation. Miscarriage is sometimes referred to as spontaneous abortion, because the medical term abortion means the ending of a pregnancy, whether intentional or unintentional. Most miscarriages occur in the first three monthns of pregnancy, between the 7th and 12th weeks of pregnancy.
How common is miscarriage?
Miscarriage is very common. Because many or even most miscarriages occur so early in pregnancy that a woman might not have known that she was pregnant, it is difficult to estimate how many miscarriages occur. Some experts believe that about half of all fertilized eggs die before implantation or are miscarried. Of known pregnancies (in which a woman misses a period or has a positive pregnancy test), about 10% to 20% end in miscarriage.
What causes miscarriage?
The majority of miscarriages are believed to be caused by genetic problems in the embryo that would prevent a baby from developing normally and surviving. These fatal genetic errors typically are not related to genetic problems in the mother.
In other cases, certain illnesses or medical conditions can cause miscarriage and may increase the risk of miscarriage. Mothers who have diabetes or thyroid disease are at increased risk of miscarriage. Infections that spread to the placenta, including some viral infections, can also increase the risk of miscarriage.
Causes of Miscarriage
Most early miscarriages (as many as 60% of first trimester ones) will remain unexplained. It is usually assumed these losses are genetic, where the chromosomes simply did not replicate correctly. Many people will assume that something that happened recently, such as an illness, fall, or exposure to something will have caused the miscarriage. This is rarely true, since by the time a miscarriage is diagnosed or begins, the baby has been lost for quite some time. Hopefully this section will help you understand the causes
There are several categories of miscarriage causes:
Sexually transmitted infections
Hormones
Chromosome Defects
Physical Problem with the Uterus or Cervix
Immune Disorders
Premature Rupture of Membranes and Early Labor
Other
Unknown
Blighted Ovum, Ectopic Pregnancy, Molar Pregnancy, and Stillbirth
There are a number of things that are not on the list above, even if you heard they cause miscarriage, because they are not documented causes of a loss.
Hormones
When we talk about a hormone problem, you have likely miscarried in less than 10 weeks. After that, the placenta has taken over hormone production and any normal deficiency you have is not a factor. Low progesterone, the most common problem, is not as easy to treat as you might hope. Progesterone suppositories, while frequently prescribed, are not proven to be helpful and often actually cause a nonviable pregnancy to last longer than it should.
The only situation where progesterone is a sure solution is with a luteal phase defect, where the corpus luteum, which is formed along with egg at ovulation, does not produce the hormones needed to sustain a pregnancy. For most women, however, this is usually not an every-month problem. Usually the situation rights itself with the next egg and the next corpus luteum. This problem, if it is a permanent one, can be diagnosed through two separate endometrial biopsies. Progesterone must be started 48 hours after ovulation to work. By the time you have missed a period, it is too late to save a pregnancy with a luteal phase defect. 5
Low progesterone, however, is usually a symptom of an nonviable pregnancy, and not thecause. Doctors often prescribe progesterone suppositories out of patient pressure when the hormone levels are low, but their use is controversial and usually completely ineffective. A common treatment for a suspected progesterone problem is Clomid, a pill taken for five days early in your cycle to rev up your hormone production. Not everyone is a candidate for Clomid, and 25% of women will have decreased cervical mucus, which can actually make you less fertile. See the Sperm Meets Egg Plan for more information.
Other hormone problems may be created when you have an untreated thyroid disorder. Your thyroid function can easily be tested, and this problem is very treatable.
Chromosome Defects
There are many factors that come in to play when the egg and sperm unite and form that first cell. Even if both the egg and sperm come with perfect chromosomes, the first few cell divisions can see an abnormality crop up that would certainly be devastating. Chromosome defects that cause a newly fertilized egg to die can account for as much as 60 percent of early miscarriages.
You can usually find out if you had a baby with a chromosome problem through testing tissue from the miscarriage. This must be done RIGHT AWAY when the tissue comes out or the cells cannot grow and the test won’t work. If this is your first miscarriage, however, do not go to great lengths to save tissue. Very few doctors will test it, and a chromosomal cause for the miscarriage will be assumed without testing.
Even when you have a D&C and the doctor sends the tissue immediately, the test still might not work. (Mine didn’t.) But if you do find your baby had a chromosome defect, find a small measure of comfort in knowing that although you lost this one precious baby, the chances of it happening again are extremely small. Another threshold will be crossed, however, at age 35. At that point, your eggs will begin to age, and your odds of a chromosomal miscarriage will begin increasing dramatically.
After the 2nd trimester begins, the number of miscarriages caused by genetic factors drops to less than 10 percent.3 If you have had several miscarriages in a row, then your odds of this being your problem are quite low, about 7%.42
Physical Problem with the womb or neck of the womb
Some women have a uterus that does not have the usual shape. Others have a cervix that may be weakened by a number of causes, including multiple D&C procedures or their mother taking DES when she was pregnant (although note that DES was discontinued in 1971 and most DES daughters are leaving their childbirth years behind.) Both of these problems can cause early labor, usually during a critical period from 12-24 weeks. This cause is responsible for 12 percent of miscarriages during this time period. As the baby grows, especially during the very rapid growth spurt during this time frame, the irregularly shaped uterus may not be able to expand or the weak cervix may start to open up and let the baby out. There are treatments for both of these that are quite effective—corrective surgery on the uterus and a cervical stitch that holds the cervix closed. This problem WILL REOCCUR if not treated.
A uterine abnormality often causes a miscarriage due to early labor, but it can also cause fetal demise, which is what happened to our Casey. Sixteen weeks into my pregnancy with Emily, we had an abnormal AFP screening. Since we were near the point of the pregnancy when Casey died, naturally we were frantic. We saw a perinatologist, who discovered I had a septate uterus. When I was a fetus, the two sections of tissue that normally fuse together to form the uterus only fused on the bottom. Therefore, there is a huge wall going down the middle of my uterus. When Casey implanted, he chose the middle wall. This section, however, has little blood flow. As Casey grew and required more and more blood and nutrition, this area could not support him. Although Emily chose a better implantation spot, this problem caused her to be breech and required a c-section. While I did have the surgery to correct this problem, my next pregnancy still had complications, and I was not allowed a vaginal delivery.
Be aware that there are varying levels of septums. Some are paper-thin and simply move out of the way for the baby, causing no problems. Others, like mine, increase your chance of miscarriage significantly. Only a high-level sonogram or an HSG dye test can uncover this problem.
Others -- Infections, Age, Chronic Disease
Many infections can cause miscarriage, but they are the big ones like syphilis, mycoplasma, toxoplasmosis, and malaria. An upper respiratory infection is NOT going to cause a miscarriage, even though it may worry you to death. Viruses are the same. Normal illnesses like the common cold will not cause a problem, but AIDS and German Measles can. Infections that directly affect the uterus are bigger risk. This does NOT include yeast infections, which are extremely common in pregnancy. See the section on Premature Rupture of Membranes for more information on these infections.
There are a few common illnesses that can cause a miscarriage or fetal malformation if you get them for the FIRST TIME during pregnancy, including Chicken Pox and Fifth Disease. The vast majority of women already have immunity to these diseases, however, and should not be concerned about exposure to them during pregnancy. If you think you may not have immunity, ask your doctor to run an antibody titer to see if you have a live antibody, or only an old antibody to the disease in your blood. Only the live antibody without the old antibody present is a danger.
An infection that causes a fever of over 101 degrees Fahrenheit should be treated immediately, however. There is a small risk that prolonged fever can affect your baby. Take Tylenol to keep your fever down and stay in touch with your doctor.
Age is only a factor in miscarriage when you consider what aging can do to your body. The first and most common is with chromosomes. It is not YOU who have a problem, it is likely your egg or sperm, which have also aged. Age can, however, bring other problems such as poor health, disease, or hormonal imbalance that can make a pregnancy harder to sustain. You don’t start seeing these problems in great numbers, however, until after 40.
Health problems in the mother can create problems with the pregnancy. Diabetes, heart problems, and thyroid disorders are just a few that may complicate the pregnancy. Having these does NOT mean you will certainly have a miscarriage. You will simply have to be more careful and make sure your treatments are adapted if needed during pregnancy.
The Unknown
Typically do not cause a miscarriage. The baby is well protected in its amniotic sac, surrounded by fluid, and even a hard blow to the abdomen will likely only rock it. Most women who have a car accident, even with a certain amount of trauma, have their babies just fine.
The hardest thing to accept is no reason at all. You live in fear, wondering if the same terrible cause of your first baby’s death will cause another one to die. You scarcely dare to try again. I have been in this situation and I tossed my doctor’s statistics aside. I had already been on the wrong side of the statistics; I didn’t care for anymore. But I do know this. One miscarriage hardly raises your chances to miscarry again at all. You are simply back at square one. Try to put the risk as far back in your mind as possible and enjoy another pregnancy. But I understand if you can’t.
Ectopic Pregnancy(pregnancy outside the womb)
Is a normal fertilized egg that gets stuck in the fallopian tube (although occasionally it will fall into the abdominal cavity) and implants there. This type of pregnancy cannot survive and puts the mother at great risk for severe hemorrhaging and possibly even death as the baby grows and eventually bursts the tube. When the ectopic is discovered based on pain and symptoms rather than an early ultrasound, the mother will immediately have surgery to remove the baby. Things will happen very fast, and most likely if this has happened to you, you are reading this after it is all over. If you are afraid you have an ectopic, the symptoms that you really want to watch for are: sharp, intense pain in your abdomen or possibly in your shoulder; a pregnancy test that is positive, then turns negative a few days later; and spotty red bleeding that continues day after day. Ectopics that are caught early can be treated with a cancer drug called Methotrexate, which will end the pregnancy safely and without surgery.
Ectopic are usually caused by scar tissue in the fallopian tubes that could have been caused by: previous surgery in the pelvic region, uterus, or tubes; a pelvic infection such as chlamydia or pelvic inflammatory
Stillbirth is technically any pregnancy that ends after the 20th week and the baby does not survive. Some babies die in utero and are discovered when the heartbeat is not found. The most common causes of this are: uterine abnormalities, a knot or other umbilical cord accident, infections of the lining of the gestational sac or cord, and placental abruptions that cause the placenta to pull away from the uterine wall. These babies are usually born through the induction of labor, although some babies are small enough to be taken by D&C or D&E procedures.
Other babies are lost through early labour. The causes of early labor are Premature Rupture of Membranes, uterine abnormalities that make the uterus too small to hold the baby, and an incompetent, which opens up and lets the baby out. Sometimes a stillbirth occurs during the birth, by an umbilical cord that gets pinched between the baby’s head and the cervix, or the cord wraps around the baby’s neck. Repeat stillbirths are extremely rare and are almost all related to uterine or cervix problems, which can be fixed or treated once found
What are the types of miscarriage?
Miscarriages are sometimes referred to by specific names to reflect the clinical findings or the type of miscarriage. Examples include:
· Threatened abortion: a woman may experience vaginal bleeding or others signs of miscarriage (see below), but miscarriage has not occurred
· Incomplete abortion: some of the products of conception (fetal and placental tissues) have been expelled from the uterus, but some remain within the uterus
· Complete abortion: all of the tissue from the pregnancy has been expelled
· Missed abortion: the fetus has not developed, so there is no viable pregnancy, but there is placental tissue contained within the uterus
· Septic abortion: a miscarriage in which there is infection in the fetal and pregnancy material before or after a miscarriage
How is miscarriagediagnosed?
An ultrasound examination is typically performed if a woman has symptoms of a miscarriage. The ultrasound can determine if the pregnancy is intact and if a fatal heartbeat is present. Ultrasound examination can also reveal whether the pregnancy is an ectopic pregnancy (located outside of the uterus, typically in theFallopian tube), which may have similar symptoms and signs as miscarriage. Other tests that may be performed include blood tests for pregnancy hormones, blood counts to determine the degree of blood loss or to see whether infection is present, and a pelvic examination. The mother’s blood type will also be checked at the time of a miscarriage, so that Rh-negative women can receive an injection of rho-D immune globulin (RhoGam) to prevent problems in future pregnancies.
What happens after a miscarriage?
There are no specific treatments that can stop a miscarriage, although women who are at risk and have not yet miscarried may be advised to rest in bed, abstain from sexual activity, and restrict all activity until any warning signs are no longer present. Once a miscarriage occurs, there is no treatment available. In many cases, the miscarriage will take its course, and unless there is severe pain and cramping or severe blood loss, no treatment is required. If a miscarriage does not completely clear the pregnancy tissue from the uterus, a procedure known as a dilatation and curettage (D&C) can be performed to remove the remaining pregnancy material. This treatment is used in the case of a missed abortion, for example, when the pregnancy material is not expelled from the uterus.
As mentioned above, women who are Rh-negative will receive a dose of rho-D immune globulin to prevent complications in future pregnancies.
If a miscarriage is due to infection, antibiotic treatment will be given.
Miscarriage is such a common occurrence that typically, unless known risk factors are present, no special testing is performed. For couples who have experienced more than two miscarriages, diagnostic studies to detect genetic, hormonal, or anatomical problems may be recommended. Some doctors recommend evaluation of the couple after the second miscarriage, particularly if the woman is over 35 years of age. Continue Reading
Medically Reviewed by a Doctor on 6/30/2014
What is the outlook for future pregnancies after a miscarriage?
Most women who miscarry go on to have a successful pregnancy. The likelihood of a miscarriage in a future pregnancy increases with the number of miscarriages a woman has had. In general, the risk of a second miscarriage in women who have had a previous miscarriage is about 15%. The risk is about 30% in women who have had two miscarriages. Most women will have their menstrual within 4 to 6 weeks after a miscarriage. Your doctor can advise you when you may start conceive again. While it is possible to conceive again after your menstrual period has returned, some doctors advise waiting a bit longer, such as another menstrual cycle or more, to provide enough time for physical and emotional recovery.
Can miscarriage be prevented?
There is no evidence that bed rest can help prevent miscarriage, but women who have vaginal bleeding during pregnancy are often advised to rest and limit sexual activity until there are no more potential signs of miscarriage. It is possible that some risk factors for miscarriage can be minimized by maintaining a healthy weight and avoiding the use of alcohol, illicit drugs, or tobacco. Screening for and treatment of any sexually-transmitted diseases (STDs) can also reduce the risk of a miscarriage. Avoidance of sports such as horseback riding or skiing can reduce your risk of trauma to the uterus. In most instances, however, the cause of a miscarriage is outside of the woman’s control.
For further information visit the EFSTH, number of government clinics throughout the country, number of NGO and private clinics E mail azadehhassan@yahoo.co.uk. Text to 002207774469/3774469
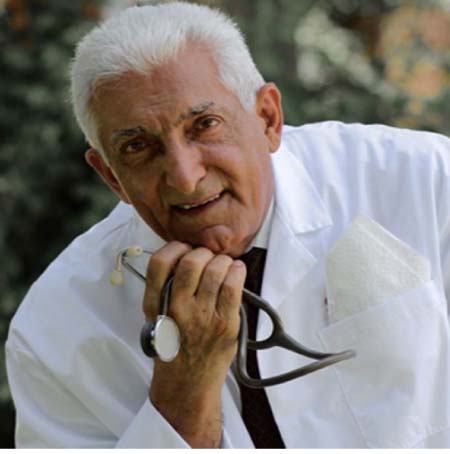
Author DR AZADEH Senior Lecturer in Obstetrics and Gynaecology at the University of the Gambia, Clinical Director of Medicare Clinic Health services.

